A rapid heartbeat – Warning sign of arrhythmia

A rapid heartbeat is a condition in which the heart beats faster than regular rates. Sometimes, it is normal for heart rates to temporarily rise during exercise, physical exertion or as a response to normal physiological stress or trauma. However, it can substantially result from a wide range of diseases and disorders. If a rapid heart rate presents, medical assistance provided by a cardiologist must be sought immediately in order to get it diagnosed and treated in a timely manner before the condition progresses. If it is left untreated, tachycardia can disrupt heart function, resulting in serious complications, including heart failure and sudden cardiac arrest.
Get to know a rapid heartbeat
Normal hearts beat 60 – 100 times every minute. When the heart beats more than 100 times each minute, that is considered a rapid heartbeat or tachycardia. A rapid heartbeat is noticed by the feeling of the heart which is pounding or fluttering much faster than normal. Tachycardia is caused by the disruptions to the normal electrical impulses that control the rate of heart’s pumping action. In addition to abnormal heart rates, irregular heart rhythms can also be a potential sign of cardiac arrhythmias.
Contributing causes to a rapid heartbeat
Numerous possible causes can induce a rapid heartbeat. These causes are divided into:
- External factors
- Dehydration
- Heavy blood loss or excessive bleeding induced anemia
- Inadequate sleep
- Infections and high-grade fever
- Thyrotoxicosis and hyperthyroidism defined as an excess of thyroid hormone in the body
- Severe diarrhea that leads to electrolyte imbalance
- Obstructive sleep apnea (OSA)
- Certain medications
- Illicit drugs or substances that stimulate the heart
- Stimulant-containing beverages e.g. tea, coffee, soft drinks, energy drinks and alcohol.
- Cardiovascular factors
- Acute myocardial infarction or a heart attack – a life-threatening condition when blood flow decreases or stops to a part of the heart, causing damage to the heart muscle.
- Hypertrophic cardiomyopathy –a disease in which the heart muscle becomes abnormally thick or hypertrophied.
- Congenital heart diseases – defined as heart problems with the heart’s structure that exist since birth.
- Valvular heart disease – defined as heart disease involving one or more of the four valves of the heart.
- Hypertension
- Certain conditions caused by electric abnormalities, e.g. supraventricular tachycardia (SVT), Wolff-Parkinson-White Syndrome (WPW) and atrial fibrillation (AF).
A rapid heartbeat potentially indicates cardiac arrhythmia
Many different types of rapid heartbeat, faster than 100 beats per minute, can indicate cardiac arrhythmia with or without irregular heart rhythm. They are grouped according to the part of the heart responsible for the fast heart rate and cause of the abnormally fast heartbeat, including:
- Supraventricular tachycardia (SVT): Supraventricular tachycardia is a fast heart rate arising from abnormal electrical activity in the upper chambers of the heart (atrium). During an episode of SVT, the heart normally beats at least 150 times per minute.
- Ventricular tachycardia (VT): Ventricular tachycardia (VT) is also a fast heart rate starting in the heart’s lower chambers, called the ventricles. VT is defined as 3 or more heartbeats in a row, at a rate of more than 120 beats per minute. If it lasts for longer than a few seconds at a time, it can become life-threatening.
- Sinus tachycardia: Sinus tachycardia is characterized by an increase in the rate of electrical impulses arising from the sinoatrial node. During an episode of sinus tachycardia, the heart rate normally ranges between 100-150 beats per minute.
Warning signs of cardiac arrhythmia
Noticeable arrhythmia symptoms often include:
- Palpitations defined as a fluttering, rapid heartbeat or pounding in the chest.
- Lightheadedness, dizziness, fainting (syncope) or near fainting
- Chest pain or tightness
- Fatigue, weakness or feeling tired easily
- Breathing difficulties, e.g. shortness of breath
- Difficulty walking, e.g. the feeling of facing air turbulence while walking
If suddenly or frequently experiencing any of these signs and symptoms at a time, it is highly recommended to seek urgent medical care.
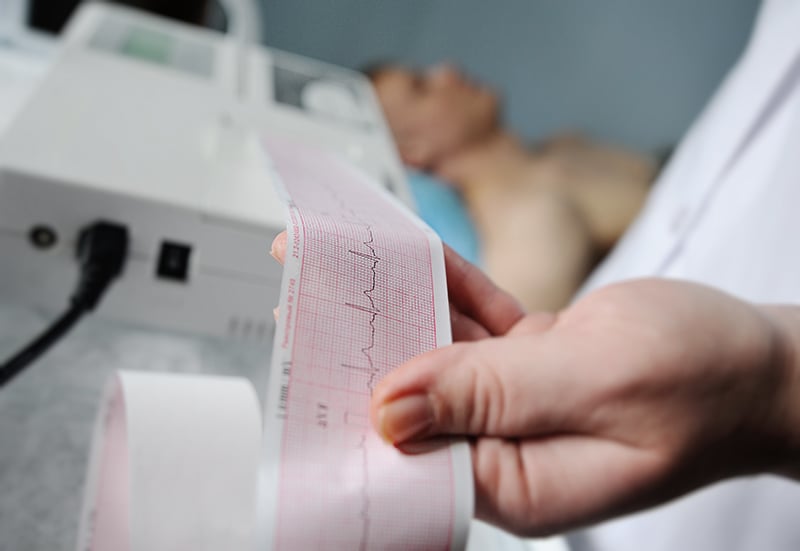
Diagnosis of cardiac arrhythmia
To diagnose a cardiac arrhythmia and rule out other conditions with similar manifestations, medical history taking and a comprehensive physical examination will be conducted by the cardiologist. In addition to blood tests, heart-monitoring tests specific to cardiac arrhythmia need to be performed. These may include:
- 12-Lead Electrocardiography (ECG or EKG): An EKG as a standard test is used to monitor heart’s rhythm and electrical activity. During an EKG, sensors or electrodes are attached to the chest and the limbs to detect the electrical activity of the heart. It measures the timing and duration of each electrical phase in the heartbeat. An EKG is often used in patients who present with irregular heartbeats for a period of time before arriving in the hospital. Moreover, it can be used for annual cardiac screening and health check-up among healthy people who have shown no abnormal signs and symptoms.
- Holter Monitoring: It is a portable EKG device that can be worn to record the heart’s rhythm and electrical activity throughout 24-48 hours. The device can detect abnormal heart rhythms despite the absence of abnormal signs or symptoms. It is often recommended for patients who regularly develop short episodes of cardiac arrhythmia everyday or almost everyday.
- Cardiac Event Recorder: A cardiac event recorder is a battery-powered portable device, looking similar to a mobile phone. It is used to tape-record the heart’s electrical activity when the patient exhibits symptoms. For sporadic arrhythmia, the patient needs to keep this portable ECG device available, attaching it to the chest wall and pressing a button while having symptoms. After pressing a button, EKG results will be recorded and sent by telephone to a receiving center or to the hospital, enabling the cardiologist to check heart rhythm at the time of symptoms. Although it is convenient, this device is only suitable for patients who occasionally experience cardiac arrhythmia symptoms only 2-3 times/month. While cardiac event recorder is useful in patients with intermittent palpitations, it has no indication to detect syncope.
- Implantable Loop Recorder (ILR): The implantable loop recorder is a subcutaneous device (usually the size of an USB flash drive) used for diagnosing heart rhythm disorders. The device is implanted under the skin in the left chest area to continually record the heart’s electrical activity and detect abnormal heart rhythms. This implantable heart-monitoring device is advised for patients who infrequently exhibit moderate to severe symptoms, such as syncope with unknown cause.
- Exercise Stress test (EST): An exercise stress test is a screening tool used to identify potential problems with heart rate, rhythm and blood flow that may predispose people to arrhythmia and other cardiovascular conditions, such as acute myocardial infarction. It shows how the heart works during physical activity or exertion. This test is often used in patients presenting with chest pain or discomfort, feeling tired easily or palpitations with unspecified cause.
- Echocardiography: Echocardiography uses sound waves to create moving pictures of the heart. It reveals the anatomy (including size and shape) and function of the heart chambers, heart valves and heart muscles. The echocardiography can detect a wide range of cardiac diseases, for instance, hypertrophic cardiomyopathy, Cardiomegaly or an enlarged heart, valvular heart diseases (e.g. valvular stenosis or valvular regurgitation) and atrial septal defect (ASD).
- Electrophysiological study: An electrophysiological study is a test used to evaluate the heart’s electrical system and to check for abnormal heart rhythms. In this test, a thin, flexible tubes (catheters) tipped with electrodes are threaded through the blood vessels to several spots within the heart. Once in place, the electrodes can map the spread of electrical impulses through the heart. In addition, the electrodes can stimulate the heart to beat at rates that may trigger a cardiac arrhythmia, allowing the cardiologist to see the origin of the arrhythmia. Nevertheless, this test is only considered when the other tests are inapplicable.
Treatment of cardiac arrhythmia
Treatment is often required if the arrhythmia causes significant symptoms putting the patients at risk of a more serious arrhythmia or arrhythmia complications. However, treatment of cardiac arrhythmia may vary among individuals, depending on type of arrhythmia and its severity as well as each patient’s condition.
- Anti-arrhythmic medications: For many types of tachycardia, anti-arrhythmic medications are often prescribed to control heart rate or restore a normal heart rhythm. The medications aim to minimize the chance of recurrence and mitigate complications while reducing disease severity that can potentially lead to death.
- Electrical cardioversion: Electrical cardioversion delivers electrical shocks to the heart through electrodes placed on the chest. The current affects the electrical impulses in the heart, resulting in a restoration of a normal rhythm.
- Radiofrequency Catheter Ablation (RFCA): In this procedure, one or more catheters are threaded through the blood vessels in the groin, arm or neck to the heart. Electrodes attached at the catheter tips using heat, extreme cold or radiofrequency energy can ablate a small spot of heart tissue and create an electrical block along the electrical pathway causing cardiac arrhythmia. Advances in 3D electroanatomic-mapping technologies, such as a Carto 3D mapping system have been currently deployed in conjunction with radiofrequency catheter ablation in order to guide for the exact region that induces electrical abnormalities, allowing a safe and effective profile of radiofrequency while minimizing the risk of procedure-related complications. The overall success rate for SVT is considerably high, over 90%. Nevertheless, one of the key components to achieve successful treatment with the best possible outcome is an expert and experienced cardiologist supported by cutting-edge technology.
- Permanent pacemaker: A permanent pacemaker is an implantable device that sends electrical pulses to help the heart beat at a normal rate and rhythm. As a minimally invasive procedure, a small device is placed under the skin near the collarbone. If an abnormal heart rate is detected, the pacemaker emits electrical impulses that stimulate the heart to restore a normal rate, enabling the heart to pump the blood more efficiently throughout the body. Permanent pacemakers are used to treat bradycardia, an abnormally slow heart rate of less than 60 beats per minute. In addition, pacemakers are also used to treat syncope (unexplained fainting spells) and heart failure.
- Automated Implantable Cardioverter-Defibrillator (AICD): An AICD is a battery-powered device implanted under the skin near the collarbone. This device continuously monitors heart rhythm and electrical system. Once it detects an abnormal heart rhythm generated from the lower chambers of the heart (e.g. ventricular tachycardia or ventricular fibrillation), it sends out low- to high-energy shocks to reset the heart to a normal rhythm. The device is therefore capable of correcting most life-threatening cardiac arrhythmias, especially those that can lead to sudden cardiac arrest. It is often recommended for patients who have a weakened heart muscle and cardiac arrhythmias caused by the lower chambers of the heart.
- Cardiac Resynchronization Therapy (CRT): Cardiac resynchronization therapy helps the heart to beat at the right rate and rhythm. It uses a pacemaker to restore the normal pattern of the heartbeat by coordinating the upper heart chambers and the lower heart chambers. Cardiac resynchronization therapy is a modality of cardiac pacing used in patients with systolic dysfunction who pose a high risk of heart failure.
Prevention of cardiac arrhythmia
In order to prevent cardiac arrhythmia and other heart diseases, it is important to live a heart-healthy lifestyle, including:
- Having an annual health check-up and cardiac screening as recommended by the cardiologist.
- Getting enough sleep
- Eating a heart-healthy diet while limiting alcohol and avoiding smoking
- Staying physically active and maintaining a healthy weight
- Drinking adequate water
- In case that the patients have other underlying conditions, diabetes, hypertension and dyslipidemia, medications to control these diseases must be strictly taken as prescribed along with regular follow-up visits.
Despite the fact that cardiac arrhythmia can strike anyone at any age, it is frequently found in patients aged over 65 who have had other preexisting conditions. It is crucial to seek urgent medical assistance if warning signs and symptoms of cardiac arrhythmia exhibits, including a fluttering in the chest or a racing heartbeat, fainting or near fainting, dizziness, chest pain or discomfort and shortness of breath. If it is left untreated, potentially life-threatening complications, such as stroke and heart failure might further develop. Under close supervision of an expert cardiologist, an early and accurate diagnosis results in effective treatments in a timely manner before the condition severely progresses.

