Keeping fit and preventing heart failure

Sudden cardiac arrest in sports as a tragic event is the leading cause of premature death in competitive athletes. During sports participation or exercise, sport-related cardiac sudden deaths have been occasionally reported despite low incidences worldwide. Sports-related sudden cardiac arrest can even cast a negative light on sports and exercise in general, therefore obscuring the health benefits of regular exercise. The answer remains unclear why this life-threatening condition could suddenly kill athletes who had never presented with any signs and symptoms of cardiac disease. The program on cardiac screening and other measures recommended by the expert cardiologist to prevent sudden cardiac death is extensively considered an important key.
What are the causes of sports-related sudden cardiac arrest in athletes?
By recent US statistics, sudden cardiac death is one of the most common medical causes of death in athletes during participation in sports, with an incidence of approximately 1 in 50,000 athletes. The incidence seems to be higher, up to 1 in 5,000, during basketball competitions. The risks and causes of sudden cardiac death widely vary based primarily upon the athlete populations. Sudden cardiac arrest is more common in men than women. Athletes aged over 35 years pose a risk of death caused by sudden cardiac arrest up to 5%, depending on the individual’s health conditions. Causes of sudden cardiac arrest during sports participation often include:- Hypertrophic cardiomyopathy – a disease in which the heart muscle (myocardium) becomes abnormally thick (hypertrophied). The thickened heart muscle in the left bottom chamber of the heart (left ventricle) becomes stiff and makes it harder for the heart to pump blood effectively throughout the body. The thickened heart muscle makes it harder for the heart to pump blood sufficiently to the rest of the body. Genetic mutations cause approximately 30% of hypertrophic cardiomyopathy cases, knows as familial hypertrophic cardiomyopathy. The genetic risk is passed from one generation to the next by dominant-acting mutations in genes governing the heart muscle structure. Familial hypertrophic cardiomyopathy is more common in African athletes compared to other ethnicities. Nevertheless, the heart muscle typically becomes thicker in athletes without clinical abnormalities. The undiagnosed athletes have irregular heart rhythm aggravated by vigorous exercise, which significantly increases the risk of sudden cardiac death.
- Myocarditis – an inflammation of the heart muscle (myocardium). Myocarditis disrupts heart muscle and heart’s electrical system, resulting in reduced heart ability to pump and leading to abnormal heart rhythms. Common cause of myocarditis is viral infections. Physical exertion can intensively provoke the left ventricle to work harder, causing abnormal heart rhythms and even sudden cardiac arrest. Therefore, athletes diagnosed with probable or definite myocarditis must not participate in sports while inflammation is present.
- Exercise-induced arrhythmia – a type of arrhythmia that is aggravating by exercise. During participating in sports competitions or training, athletes lost water and electrolytes as a consequence of sweating. These electrolytes play a significant role in conducting the electrical impulses in the heart. Electrolyte disturbance results in detrimental effects to the heart, contributing to electrical imbalance and arrhythmia development. The most common symptoms of an exercise-induced arrhythmia include a fluttering sensation in the chest and racing or lowered heart rate. In many cases, arrhythmia is undiagnosed since no clinical sign, or symptom shows up, especially in younger athletes aged below 35. Due to a lack of awareness, young athletes might overlook regular cardiac screening.
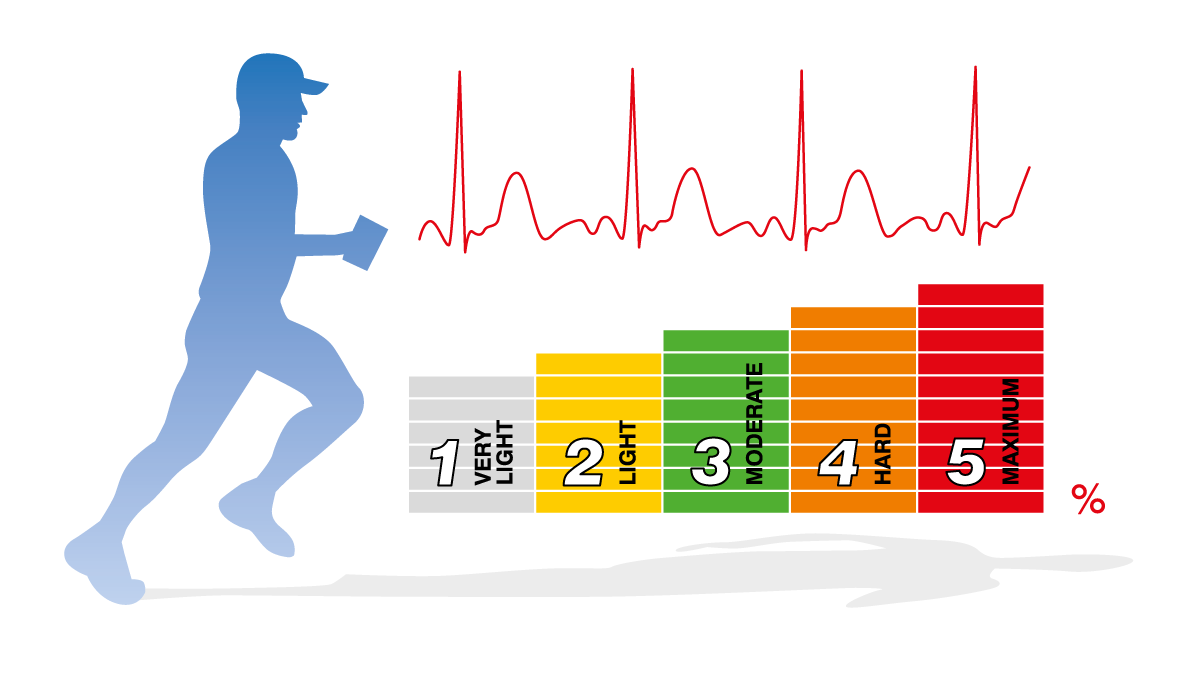
Heart rate training zones
Heart rate training zones help to train at the required intensity according to the current health condition while not unintentionally pushing the body and the heart over the limit. There are five heart rate zones based on training intensity, regarding Maximum Predicted Heart Rate or MPHR.
- Zone 1 (Very light, 50-60 % of MPHR): Improving overall health and metabolism with easy breathing. This training zone is recommended for novice exercisers, weight management and active recovery.
- Zone 2 (Light, 60-70 % of MPHR): Improving endurance with easy breathing, low muscle load and light sweating. It helps to remove excess fat, which is beneficial to the heart and lungs.
- Zone 3 (Moderate, 70-80 % of MPHR): Improving aerobic fitness with moderate sweating. This training zone is recommended for active exercisers.
- Zone 4: (Hard, 80-90 % of MPHR): Increasing maximum performance capacity with more muscular fatigue and heavy breathing. This zone is suitable for athletes or physically active people.
- Zone 5: (Maximum, 90-100 % of MPHR): Increasing maximum sprint race speed with exhausting breathing and muscular fatigue. This zone is only recommended for professional athletes with athletic training background.
Getting fit before striking the games
Before a kick-off, pre-participation screening, including cardiac screening tests and physical fitness assessment, aims to identify cardiovascular diseases, musculoskeletal problems, and other exercise-aggravated medical conditions. A comprehensive pre-participation screening program conducted by sports medicine physicians and cardiologists include:
- Medical history and physical examination: Medical history and physical examination are defined as the systematic medical practice of evaluating athletes before sports participation to identify or raise suspicion of any abnormalities that might undergo sudden cardiac death.
- Electrocardiography (EKG): EKG is used to check heart’s rhythm and electrical activity. Interpretation of the EKG of young athletes, aged below 35 can help identify their cardiac abnormalities that put them at greater risk of sudden cardiac arrest, resulting in a reduction in death rates up to 90% among young athletes.
- Exercise stress test: An exercise stress test is a screening tool used to identify potential problems with heart rate, rhythm and blood flow that may predispose athletes to sudden death. It shows how the heart works during physical activity or exertion. The test can screen for coronary artery disease or CAD (thickening and narrowing of the coronary arteries) presenting with the blockage greater than 70 percent which severely limits blood flow.
- Cardiac magnetic resonance imaging (Cardiac MRI scan): Cardiac MRI scan can detect cardiac diseases by evaluating the anatomy and function of the heart chambers, heart valves and the surrounding structures including major coronary and pulmonary blood vessels. The contrast medium used during cardiac MRI scanning highlights the blood vessels to examine the blood flow or perfusion to the heart. In addition, a cardiac MRI scan can be used to identify myocarditis and myocardial hypertrophy caused by prolonged and increased stress on the heart.
- Coronary Artery Calcium Scan (CAC): CAC is an imaging test used to detect the atherosclerotic plaque that forms on the artery walls of the heart, leading to coronary artery disease. It predicts the likelihood (presented as predictive value) of a myocardial infarction or heart attack caused by atherosclerotic plaque. The test is often recommended for people aged over 40 as their risks of developing coronary artery disease substantially increase.
Warning signs that athletes should seek immediate medical assistance are feeling very tired easily, fluttering sensation in the chest or irregular heartbeat, fainting and shortness of breath. If these abnormalities are left undiagnosed or untreated, they can be a potential cause of cardiac sudden death among athletes, regardless of age, gender and ethnicity.
Automated External Defibrillators (AEDs) as onsite life-saving devices
Automated external defibrillators (AEDs) are portable, life-saving devices designed to revive people from sudden cardiac arrest occurring when there is a disruption in the heart’s electrical activity. AEDs analyze the heart rhythm and deliver a therapeutic electric shock to the heart, enabling the heart to return to its normal rhythm. AEDs are mobile and essential to be placed in public venues including sport fields and stadiums. The location of the AED should be well-marked and known among athletic staff. It is critical that the location must be close enough to the venue that it takes no longer than 3-5 minutes from the time of collapse to the first administered shock. If someone experiences sudden cardiac arrest, step-by-step instructions for prompt assistance include:
- Assessment prior to assistance: When a potential cardiac arrest patient is identified, the first step is to assess the surrounding environment whether it is safe and suitable for further resuscitation.
- Calling emergency services for assistance.
- Providing cardiopulmonary resuscitation (CPR): CPR should be immediately provided once no response shown from the patient. CPR combining effective chest compressions with artificial ventilation in an effort to manually resuscitate the patient must constantly continue until AED or emergency service arrives at the scene.
The significant role of the pre-participation screening is to evaluate the health of professional athletes to optimize safe sports participation. Pre-participation cardiovascular screening aims to provide medical clearance for participation in competitive sports through routine and systematic evaluations. Early detection of athletes at risk for sudden cardiac arrest can extensively minimize the chance of death. For physically active people or amateurs, regular health check-ups are highly advised to track any abnormalities in a timely manner before disease develops.

